PakAlumni Worldwide: The Global Social Network
The Global Social Network
India Lags Sub-Saharan Africa in Public Hygiene
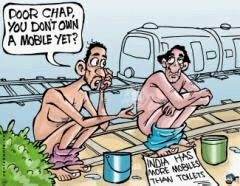
India(638m) is followed by Indonesia (58m), China (50m), Ethiopia (49m), Pakistan (48m), Nigeria (33m) and Sudan (17m). In terms of percentage of each country's population resorting to the unhygienic practice, Ethiopia tops the list with 60%, followed by India 54%, Nepal 50%, Pakistan 28%, Indonesia 26%, and China 4%.
18 percent of urban India still defecates in open while the percentage of rural India is as high as 69 percent of the population. It is the key reason why India carries among the highest infectious disease burdens in the world.
The number of open defecators in rural India alone is more than twice those in the whole of sub-Saharan Africa, according to a report by DFID, the UK's Department for International Development.
The World Bank has estimated that open defecation costs India $54 billion per year or $48 per head. This is more than the Government of India’s entire budget for health.
The UNICEF report says that with only four more years to go until 2015, a major leap in efforts and investments in sanitation is needed to reach the targets of Millennium Development Goals.
After the embarrassing headlines, it appears that Minister Ramesh is ready to step up the efforts to improve sanitation. He is quoted by Times of India as saying that "we are going to focus now on `nirmal gram abhiyan' -- today 25,000 nirmal grams are a tiny fraction of 6 lakh villages. These nirmal grams are in Maharashtra and Haryana. Maharashtra is a success of social movements while Haryana an example of determined state government action."
Here's a video clip of Indian environment minister Jairam Ramesh saying "if there was a Nobel Prize for dirt and filth, India would win it hands down":
Related Links:
Haq's Musings
Fixing Sanitation Crisis in India
Food, Clothing and Shelter in India and Pakistan
Heavy Disease Burdens in South Asia
Peepli Live Destroys Indian Myths
India After 63 Years of Independence
Poverty Across India 2011
India and Pakistan Contrasted
-
Comment by Riaz Haq on February 14, 2021 at 9:52am
-
White Tiger Movie Review
https://www.washingtonpost.com/goingoutguide/movies/the-white-tiger...
There’s a sense of snarling menace implicit in “The White Tiger,” a subversive, sharp-toothed dramedy of upward social mobility by writer-director Ramin Bahrani (“99 Homes”), based on Aravind Adiga’s best-selling 2008 novel, which won the Man Booker Prize. It’s not just in the title, a metaphorical moniker for uniqueness slapped on the film’s ambitious protagonist, a canny but impoverished low-caste Indian named Balram (Adarsh Gourav), as a child. It’s there, lurking in every shadow of this dark rags-to-riches tale itself: a coiled threat to the traditional world order of haves and have-nots, just waiting to pounce.
After the opening scene, set in a car careening through the streets of Delhi at night — a short, alarming prologue that is quickly interrupted by Balram’s narration, framed somewhat preposterously as an email he’s composing to Chinese Premier Wen Jiabao on the eve of his 2010 visit to India — the film gets down to business. Told mostly in flashback, “Tiger” follows Balram’s rise from poverty to become the No. 2 chauffeur for a rich, corrupt landlord known as the Stork (Mahesh Manjrekar) and his son Ashok (Rajkummar Rao).
It isn’t long that he’s No. 2. Balram soon supplants the Stork’s top driver (Girish Pal) when he reveals that the longtime employee — or servant, in the parlance of the film — is a Muslim. (The Stork hates Muslims.) Soon Balram is making money in side hustles that involve submitting fake invoices to his boss for unnecessary repairs, and siphoning gas to sell on the streets, all the while ingratiating himself with the Western-educated Ashok and his American-raised wife, a chiropractor named Pinky (Priyanka Chopra Jonas). Both of them are progressive enough to treat Balram not as their servant but their pal — until it no longer serves them, that is.
Such polarization and inequality — Balram casts it as another dichotomy: an India of darkness, and an India of light — isn’t unique to his country. And as the blithely clueless cheerfulness of film’s antihero gradually curdles to cunning connivance, so does the narrative’s black comedy congeal, taking on a tone that is less jokey than sickening. (Balram cracks wise throughout the film, saying at one point, about the world’s largest democracy: “If I were in charge of India, I’d get the sewage pipes first, then the democracy.”)
-
Comment by Riaz Haq on July 4, 2021 at 8:21pm
-
#Fake #vaccines administered in #India. #Medical scams are nothing new in India, where, during the country’s mammoth outbreak this spring, profiteers targeted vulnerable #COVID19 patients with fake drugs and oxygen. #Modi #BJP #fraud #pandemic https://www.nytimes.com/2021/07/04/world/asia/india-covid-vaccine-s...
As India intensifies its vaccination effort amid fears of another wave of the coronavirus, officials are investigating allegations that perhaps thousands of people were injected with fake vaccines in the financial capital, Mumbai.
The police have arrested 14 people on suspicion of involvement in a scheme that administered injections of salt water instead of vaccine doses at nearly a dozen private vaccination sites in Mumbai over the past two months. The organizers, including medical professionals, allegedly charged between $10 and $17 per dose, according to the authorities, who said they had confiscated more than $20,000 from the suspects.
“Those arrested are charged under criminal conspiracy, cheating and forgery,” said Vishal Thakur, a police officer in Mumbai.
More than 2,600 people came to the camps to receive shots of the Oxford-AstraZeneca vaccine, manufactured and marketed in India as Covishield. Some said that they became suspicious when their shots did not show up in the Indian government’s online portal tracking vaccinations, and when the hospitals that the organizers had claimed to be affiliated with did not match the names on the vaccination certificates they received.
“There are doubts about whether we were actually given Covishield or was it just glucose or expired/waste vaccines,” Neha Alshi, who said she was a victim of the scam, wrote on Twitter.
Siddharth Chandrashekhar, a lawyer who has filed a public interest lawsuit in Mumbai’s high court, described the scenario as “heartbreaking.” The court said it was “really shocking that incidents of fake vaccination are on the rise.”
Medical scams are nothing new in India, where, during the country’s mammoth outbreak this spring, profiteers targeted vulnerable Covid patients with fake drugs and oxygen. The police in West Bengal state are also investigating whether hundreds of people, including a local lawmaker, received fake vaccines there.
India has administered more than 340 million vaccine doses, but less than 5 percent of the population is fully vaccinated, according to the Our World in Data project at the University of Oxford. The country is reporting nearly 50,000 new cases daily and nearly 1,000 Covid deaths, numbers that are far lower than two months ago, although experts have always believed India’s official tallies to be vastly undercounted.
On Saturday, the pharmaceutical company Bharat Biotech reported that its Covaxin shot — the other vaccine in wide use in India — was 77.8 percent effective in preventing symptomatic illness, according to the results of a late-stage trial. Those results were published online but have not been peer-reviewed.
-
Comment by Riaz Haq on March 25, 2022 at 12:47pm
-
Patients are flocking to #India for surgery but "Indian #medical #tourism lacks effective regulations to govern the sector, which leaves it unorganized and lacking in monitoring". The quality of the services provided by these agents is not regulated. https://www.bbc.com/news/business-60569647
"India has the largest pool of clinicians in South Asia," explains Dinesh Madhavan, President of Group Oncology at International Apollo Hospital Enterprises.
"We are uniquely positioned thanks to our hospitality and rich culture, combined with modern as well as traditional medicine and therapy," he says.
And it's not just treatment for medical conditions like cancer. There has also been a sharp rise in patients arriving in India for cosmetic surgery procedures such as liposuction (removal of body fat) or hair grafts for baldness.
"We get patients from the US, Africa and Gulf regions," says Dr Satish Bhatia, a dermatologist and cutaneous surgeon in Mumbai. Dr Bhatia says he sees many flight attendants, looking for quick, non-invasive cosmetic procedures such as dermal fillers or Botox.
Dr Bhatia says that, on average, the price of most cosmetic procedures in the US, Europe and the Middle East are at least 50% higher than if done in India.
Like much travel, medical tourism ground to a halt during the pandemic, but Dr Bhatia says business is picking up again and he is confident it will continue to grow.
However, this boom in overseas patients has its downsides.
"There is a mushrooming of new aesthetic clinics all around India. Sadly, this also attracts unqualified and untrained doctors wanting to make easy money," says Dr Bhatia.
Always research your doctor's credentials and experience before fixing an appointment, he advises.
Patients should also make sure there are adequate arrangements in place for aftercare, says Dr Shankar Vangipuram, senior consultant, radiation oncology at the Apollo Cancer Centre in Chennai.
"Post-treatment in India - sometimes due to lack of qualified clinicians and diagnostic tools - we do face difficulty in tracking the responses and toxicities," he says.
The government meanwhile, acknowledges that the sector needs tighter regulation.
-
Comment by Riaz Haq on April 15, 2022 at 4:53pm
-
#India’s drug regulator has ignored red alerts on #COVAXIN, imperiling millions of lives. World #Health Organization warned #UN agencies against procuring Covaxin, India’s indigenously developed & manufactured #COVID19 #vaccine. #Modi #Hindutva #Bharat https://www.statnews.com/2022/04/15/indias-drug-regulator-has-ignor...
Why are CDSCO and others treating Bharat Biotech with kid gloves?
The simple answer is that virtually all of India has thrown its weight behind Bharat Biotech because of Prime Minister Narendra Modi’s AatmaNirbhar policy, which broadly translates into a policy of economic self-reliance. This has meant special regulatory privileges for Covaxin, given its status as a made-in-India vaccine that was developed with the support of the Indian Council of Medical Research (ICMR).
--------
In a shocking turn of events, the World Health Organization warned United Nations agencies against procuring Covaxin, India’s indigenously developed and manufactured Covid-19 vaccine, just five months after granting approval to the made-in-India vaccine. The warning came after a WHO inspection of a manufacturing facility owned by Bharat Biotech International Ltd. revealed “deficiencies in good manufacturing practices.”
The WHO has not revealed the extent or nature of the deficiencies at Bharat Biotech’s facility; but given its recent instructions to U.N. agencies, the deficiency must have been significant from a public health perspective. Violations of current good manufacturing processes is nothing new to the Indian pharmaceutical industry. There is a sordid history of warning letters from the U.S. Food and Drug Administration documenting systematic compliance issues over the last decade. Foreign inspections all but ceased during the pandemic. Agencies such as the WHO rely on national regulatory agencies like the Central Drugs Standard Control Organisation (CDSCO), which regulates the pharmaceutical industry in India, to assess compliance before granting approval for commercial use of a drug.
This is not the first time that a foreign regulator has found problems with the manufacturing facility at Bharat Biotech that produces Covaxin. Exactly one year ago, the Agência Nacional de Vigilância Sanitária (ANVISA), Brazil’s drug regulator, pointed out serious lapses at Bharat Biotech’s manufacturing facility in India that makes this vaccine. ANVISA inspectors discovered issues with quality control at the facility that are meant to confirm that the live virus at the core of this vaccine has been inactivated.
At the time, the CDSCO remained a mute spectator to the affair and gave no assurances to the Indian public on measures it was taking to ensure that Bharat Biotech fixed these issues. It has followed the same path of silence since the WHO’s recent suspension of Covaxin’s procurement by the United Nations.
As I write this, not a single newspaper in India has been able to identify the exact nature of the deficiency the WHO raised, and few in India seem to be concerned about the implications of the WHO’s action, despite the fact that Covaxin is being administered to children in India.
-
Comment by Riaz Haq on June 1, 2022 at 7:22am
-
India wants to be the ‘pharmacy of the world.’ But first, it must wean itself from China
https://www.cnbc.com/2022/05/27/india-needs-to-fill-china-gaps-to-b...
India has embarked on an ambitious plan to cut dependence on China for key raw materials as it seeks to become self-sufficient in its quest to be the “pharmacy of the world.”
However, India’s $42 billion pharmaceutical sector is heavily dependent on China for key active pharmaceutical ingredients or API — chemicals that are responsible for the therapeutic effect of drugs.
Estimates put India’s dependence on China at as much as 90% for certain drugs.
an estimate by the Trade Promotion Council, a government supported organization, puts the figure of API dependence on China at about 85%. Another independent study carried out in 2021 points out that while India’s API imports from China are at nearly 70%, its dependence on China for “certain life-saving antibiotics” is around 90%. Some drugs that are highly dependent on Chinese APIs include penicillin, cephalosporins and azithromycin, the report said.
That may be starting to change.
Under a government scheme launched two years ago, 35 APIs began to be produced at 32 plants across India in March. This is expected to reduce dependence on China by up to 35% before the end of the decade, according to an estimate by ratings firm ICRA Limited, the Indian affiliate of Moody’s.
The production linked incentive scheme was first launched in mid-2020, when military tensions with China were at a high. The PLI program aims to incentivize companies across all sectors to boost domestic manufacturing by $520 billion by 2025.
For the pharma sector, the government has earmarked over $2 billion worth of incentives for both private Indian companies and foreign players to start producing 53 APIs that India relies heavily on China for.
Some of India’s biggest pharmaceutical companies are involved in the scheme. They include Sun Pharmaceutical Industries, Aurobindo Pharma, Dr. Reddy’s Laboratories, Lupin and Cipla.
A total of 34 products were approved in the first phase of the scheme — and distributed amongst 49 players, according to assistant vice president at ICRA Limited, Deepak Jotwani.
“The first phase will result in reduction in imports from China by about 25-35% by 2029,” Jotwani estimated.
-
Comment by Riaz Haq on October 5, 2022 at 6:52pm
-
India-made cough syrups may be tied to 66 deaths in Gambia: WHO | Business and Economy News | Al Jazeera
https://www.aljazeera.com/economy/2022/10/5/india-made-cough-syrups...
The WHO also issued a medical product alert asking regulators to remove Maiden Pharma goods from the market.
The deaths of dozens of children in The Gambia from kidney injuries may be linked to contaminated cough and cold syrups made by an Indian drug manufacturer, the World Health Organization said on Wednesday.
WHO Director-General Tedros Adhanom Ghebreyesus told reporters that the UN agency was conducting an investigation along with Indian regulators and the drugmaker, New Delhi-based Maiden Pharmaceuticals Ltd.
Maiden Pharma declined to comment on the alert, while calls and Reuters messages to the Drugs Controller General of India went unanswered. The Gambia and India’s health ministry also did not immediately respond to a request for comment.
The WHO also issued a medical product alert asking regulators to remove Maiden Pharma goods from the market.
The products may have been distributed elsewhere through informal markets, but had so far only been identified in The Gambia, the WHO said in its alert.
The alert covers four products – Promethazine Oral Solution, Kofexmalin Baby Cough Syrup, Makoff Baby Cough Syrup and Magrip N Cold Syrup.
Lab analysis confirmed “unacceptable” amounts of diethylene glycol and ethylene glycol, which can be toxic when consumed, the WHO said. The Gambia’s government said last month it has also been investigating the deaths, as a spike in cases of acute kidney injury among children under the age of five was detected in late July.
Medical officers in The Gambia raised the alarm in July, after several children began falling ill with kidney problems three to five days after taking a locally sold paracetamol syrup. By August, 28 had died, but health authorities said the toll would likely rise. Now 66 are dead, WHO said on Wednesday.
The deaths have shaken the tiny West African nation, which is already dealing with multiple health emergencies including measles and malaria.
Maiden Pharmaceuticals manufactures medicines at its facilities in India, which it then sells domestically, as well as exporting it to countries in Asia, Africa and Latin America, according to its website.
-
Comment by Riaz Haq on October 9, 2022 at 6:25pm
-
#India facing a #pandemic of #antibiotics-resistant superbugs. It is worst hit by what doctors call "antimicrobial resistance" - #antibiotic-resistant neonatal #infections alone are responsible for the deaths of nearly 60,000 newborns each year. #health https://www.bbc.com/news/world-asia-india-63059585
Things are so worrying that only 43% of the pneumonia infections caused by one pathogen in India could be treated with first line of antibiotics in 2021, down from 65% in 2016, the ICMR report says.
Saswati Sinha, a critical care specialist in AMRI Hospital in the eastern city of Kolkata, says things are so bad that "six out of 10" patients in her ICU have drug-resistant infections. "The situation is truly alarming. We have come to a stage where you are not left with too many options to treat some of these patients."
----------
At the 1,000-bed not-for-profit Kasturba Hospital in the western Indian state of Maharashtra, doctors are grappling with a rash of antibiotic-resistant "superbug infections".
This happens when bacteria change over time and become resistant to drugs that are supposed to defeat them and cure the infections they cause.
Such resistance directly caused 1.27 million deaths worldwide in 2019, according to the Lancet medical journal. Antibiotics - which are considered to be the first line of defence against severe infections - did not work on most of these cases.
Millions are dying from drug-resistant infections
India is one of the countries worst hit by what doctors call "antimicrobial resistance" - antibiotic-resistant neonatal infections alone are responsible for the deaths of nearly 60,000 newborns each year. A new government report paints a startling picture of how things are getting worse.
Tests carried out at Kasturba Hospital to find out which antibiotic would be be most effective in tackling five main bacterial pathogens have found that a number of key drugs were barely effective.
These pathogens include E.coli (Escherichia coli), commonly found in the intestines of humans and animals after consumption of contaminated food; Klebsiella pneumoniae, which can infect the lungs to cause pneumonia, and the blood, cuts in the skin and the lining of the brain to cause meningitis; and the deadly Staphylococcus aureus, a food-borne bacteria that can be transmitted through air droplets or aerosols.
Doctors found that some of the main antibiotics were less than 15% effective in treating infections caused by these pathogens. Most concerning was the emergence of the multidrug-resistant pathogen called Acinetobacter baumannii, which attacks the lungs of patients on life support in critical care units.
Hidden pandemic of antibiotic-resistant infections
"As almost all our patients cannot afford the higher antibiotics, they run the real risk of dying when they develop ventilator-associated pneumonia in the ICU," Dr SP Kalantri, medical superintendent of the hospital, says.
A new report by Indian Council of Medical Research (ICMR) says that resistance to a powerful class of antibiotics called carbapenems - it defeats a number of pathogens - had risen by up to 10% in just one year alone. The report collects data on antibiotic resistance from up to 30 public and private hospitals every year.
"The reason why this is alarming is that it is a great drug to treat sepsis [a life-threatening condition] and sometimes used as a first line of treatment in hospitals for very sick patients in ICUs," says Dr Kamini Walia, a scientist at Indian Council of Medical Research (ICMR) and lead author of the study.
-
Comment by Riaz Haq on November 3, 2022 at 8:13am
-
Necessary #Indian Drugs Prove Deadly For Dozens of Children. Deaths believed to be linked to contaminated #cough syrups in #Gambia have brought attention to loose #regulations in #India and a lack of testing capacity in poor importing nations. #health https://www.nytimes.com/2022/11/03/world/asia/india-gambia-cough-sy...
“What happened in Gambia is happening in other African countries without us even knowing,” said Michel Sidibé, the African Union special envoy for the African Medicines Agency, a new body aimed at harmonizing drug regulation across the continent.
“Most African countries don’t have testing capacities nor well-trained regulatory bodies,” Mr. Sidibé said. “The African market is very fragmented, but because of poor regulations, drugs move from one country to another.”
-------------
They had fevers, aches, runny noses, the normal stuff of childhood. The kind of illnesses for which a doctor would prescribe cough syrup.
But the children’s condition only worsened. They developed persistent diarrhea, then could no longer urinate, as their kidneys failed. The very medicines that were supposed to make them better, simple cough syrups imported from India, were instead killing them, because they turned out to be poison.
In all, 70 children in the tiny West African nation of Gambia are suspected to have died in recent months from contaminated Indian-made cough syrups. Among them was 2-year-old Muhammad Lamin Kijera, who died on Aug. 4.
“He was lively and likable — he was everybody’s friend,” said his father, Alieu Kijera, who works as a nurse at an eye clinic in Banjul, the Gambian capital. “How can they allow something like this into the country, destroying lives?”
India has taken to calling itself “the world’s pharmacy” as its drug industry has expanded rapidly, providing a lifeline to the developing world by selling medicines, many of them generics, for an array of illnesses like malaria and AIDS at prices lower than those of American or European drugs.
But the deaths in Gambia have raised alarm over what one expert called a “dangerous cocktail”: on one side, a $50 billion Indian pharmaceutical industry whose regulation has remained loose and chaotic despite repeated calamities, and on the other, poor nations with little or no way to test the quality of the medicines they import.
India’s drug industry, experts say, is rife with data fraud, inadequate testing and substandard manufacturing practices. While people around the world take Indian medicines every day without incident, the regulatory weaknesses give the country’s drug makers openings to cut corners and increase profits, experts say.
That has created a hazardous reality far more widespread than the occasional tragic cases of mass poisonings, and could shake faith in Indian medicines in the places that need them most.
----------
India is the world’s third-largest drug manufacturer by volume, producing 60 percent of global vaccines and 20 percent of generic medicines. In a sign of the world’s reliance on Indian drugs, the country’s pharmaceutical exports increased nearly 20 percent during the first year of the pandemic, reaching $24 billion, despite lockdowns that disrupted global supply chains.
As a stamp of approval for the quality of Indian medicines, officials point out that more than half of the drugs manufactured in India go to highly regulated markets — “every third pill in the U.S. and every fourth pill in Europe is sold from India,” according to the Indian Pharmaceutical Alliance.
-
Comment by Riaz Haq on December 12, 2022 at 6:01pm
-
#India still uses #asbestos. Poor #Indians use it for roofing. WHO says all asbestos types cause “lung cancer, mesothelioma, cancer of the larynx and ovary, and asbestosis [fibrosis of the lungs]”. Exposure, handling or inhaling it results in death.
https://aje.io/6v4rpw
Asbestos – a cheap, heat-resistant mineral – was once used widely in building materials all around the world. Today, it is banned in 70 countries which have deemed that this construction material is a “silent killer” since its fibres are carcinogenic.
While there are six types of asbestos, chrysotile – white asbestos – is the most common form, used especially in roofing houses.
According to the World Health Organization, all types of asbestos cause “lung cancer, mesothelioma, cancer of the larynx and ovary, and asbestosis [fibrosis of the lungs]”.
Exposure to the fibres and handling or inhaling them could also result in death.
Yet some countries like India continue trading it.
In 2011, India banned asbestos mining and asbestos waste used in ships. But it continues to trade in raw asbestos and asbestos-based products, commonly found in the roofs of houses, especially in poorer regions of the country.
According to a November 2021 report by the Indian government, between 2019 and 2020, India imported 361,164 tonnes of asbestos, a 1 percent decrease compared with 364,105 tonnes in the previous year.
The report noted that almost the entire import was chrysotile asbestos, with 85 percent of these fibres coming from Russia. About 3 percent also came from Brazil, Kazakhstan and Hungary each, and 2 percent came from Poland and South Africa respectively.
Aaron Cosbey, a development economist and head of Small World Sustainability, a consultancy, told Al Jazeera that trade goes on because commercial interests have been prioritised over human welfare.
“India’s biggest source of chrysotile asbestos – Russia – has not banned it nationally. So there is no hypocrisy; it is just bad policy, given that the WHO and 70 states worldwide have agreed that there are no safe uses for the substance,” he said.
India also exports asbestos, but its sales have decreased substantially to 1,001 tonnes between 2019 and 2020, compared with 1,112 tonnes in the previous year.
The Indian government’s November 2021 report noted that most of the exports went to Bangladesh, and 7 percent to Sri Lanka.
Gopal Krishna, an environmental lawyer and co-founder of the Ban Asbestos Network of India, said despite countries like Brazil ruling that asbestos use was unconstitutional – and Hungary, Poland and South Africa banning asbestos – India continues with its import and export.
“The trade continues because nobody in India has time to deal with health complaints when money is involved and there is a lewd relationship between the Indian government and the asbestos manufacturers in the country,” he told Al Jazeera.
“A 2012 study (PDF) was conducted by the National Institute of Occupational Health in Ahmedabad, India, surveying 1,248 workers exposed to the substance. Noting that the fibres affected only three workers, the study concluded that asbestos and its derivatives are not harmful to human health. But this study by a government body was co-sponsored by the Asbestos Cement Products Manufacturers’ Association, which lobbies for the industry, making it a conflict of interest,” he added.
Krishna said the study contradicts the UN Rotterdam Convention, which was adopted in 2004 and reviews the harmful effects of a wide range of chemicals and pesticides.
-
Comment by Riaz Haq on January 7, 2023 at 8:07pm
-
Postponing India’s census is terrible for the country
But it may suit Narendra Modi just fine
https://www.economist.com/asia/2023/01/05/postponing-indias-census-...
Narendra Modi often overstates his achievements. For example, the Hindu-nationalist prime minister’s claim that all Indian villages have been electrified on his watch glosses over the definition: only public buildings and 10% of households need a connection for the village to count as such. And three years after Mr Modi declared India “open-defecation free”, millions of villagers are still purging al fresco. An absence of up-to-date census information makes it harder to check such inflated claims. It is also a disaster for the vast array of policymaking reliant on solid population and development data.
----------
Three years ago India’s government was scheduled to pose its citizens a long list of basic but important questions. How many people live in your house? What is it made of? Do you have a toilet? A car? An internet connection? The answers would refresh data from the country’s previous census in 2011, which, given India’s rapid development, were wildly out of date. Because of India’s covid-19 lockdown, however, the questions were never asked.
Almost three years later, and though India has officially left the pandemic behind, there has been no attempt to reschedule the decennial census. It may not happen until after parliamentary elections in 2024, or at all. Opposition politicians and development experts smell a rat.
----------
For a while policymakers can tide themselves over with estimates, but eventually these need to be corrected with accurate numbers. “Right now we’re relying on data from the 2011 census, but we know our results will be off by a lot because things have changed so much since then,” says Pronab Sen, a former chairman of the National Statistical Commission who works on the household-consumption survey. And bad data lead to bad policy. A study in 2020 estimated that some 100m people may have missed out on food aid to which they were entitled because the distribution system uses decade-old numbers.
Similarly, it is important to know how many children live in an area before building schools and hiring teachers. The educational misfiring caused by the absence of such knowledge is particularly acute in fast-growing cities such as Delhi or Bangalore, says Narayanan Unni, who is advising the government on the census. “We basically don’t know how many people live in these places now, so proper planning for public services is really hard.”
The home ministry, which is in charge of the census, continues to blame its postponement on the pandemic, most recently in response to a parliamentary question on December 13th. It said the delay would continue “until further orders”, giving no time-frame for a resumption of data-gathering. Many statisticians and social scientists are mystified by this explanation: it is over a year since India resumed holding elections and other big political events.
Twitter Feed
Live Traffic Feed
Sponsored Links
South Asia Investor Review
Investor Information Blog
Haq's Musings
Riaz Haq's Current Affairs Blog
Please Bookmark This Page!
Blog Posts
Pakistani Student Enrollment in US Universities Hits All Time High
Pakistani student enrollment in America's institutions of higher learning rose 16% last year, outpacing the record 12% growth in the number of international students hosted by the country. This puts Pakistan among eight sources in the top 20 countries with the largest increases in US enrollment. India saw the biggest increase at 35%, followed by Ghana 32%, Bangladesh and…
ContinuePosted by Riaz Haq on April 1, 2024 at 5:00pm
Agriculture, Caste, Religion and Happiness in South Asia
Pakistan's agriculture sector GDP grew at a rate of 5.2% in the October-December 2023 quarter, according to the government figures. This is a rare bright spot in the overall national economy that showed just 1% growth during the quarter. Strong performance of the farm sector gives the much needed boost for about …
ContinuePosted by Riaz Haq on March 29, 2024 at 8:00pm
© 2024 Created by Riaz Haq.
Powered by
![]()
You need to be a member of PakAlumni Worldwide: The Global Social Network to add comments!
Join PakAlumni Worldwide: The Global Social Network